
What Is Macular Degeneration An Easy To Understand Guide
Macular degeneration is a surprisingly common eye condition, especially as we get older. It targets the very center of your vision, leaving your peripheral (side) vision totally fine. This is why it's often called Age-related Macular Degeneration (AMD). The condition damages a tiny but critical spot near the center of your retina called the macula, which is responsible for seeing fine details with sharp clarity.
A Simple Guide to Macular Degeneration
Think of your eye as a high-tech camera. The macula is its most powerful sensor, the part that captures crisp, high-definition images right in the middle of your view. When macular degeneration kicks in, it’s like that central sensor is starting to wear out. It doesn't lead to complete blindness, but it can create a blurry or dark spot right in your line of sight.
This loss of central vision can really throw a wrench in day-to-day life. Things you take for granted, like recognizing a friend's face across the street, reading the fine print on a prescription bottle, or even driving, suddenly become a huge challenge. Your side vision is still working, but the crucial details right in front of you start to vanish.
To give you a quick and clear overview, here’s a simple breakdown of the condition.
Macular Degeneration At A Glance
| Key Aspect | Brief Explanation |
|---|---|
| What it is | An eye disease that damages the macula, causing loss of central vision. |
| Main Type | Age-related Macular Degeneration (AMD). |
| Primary Impact | Blurs or creates dark spots in the direct line of sight. |
| Effect on Daily Life | Makes detailed tasks like reading, driving, and recognizing faces difficult. |
| Does it cause blindness? | No, it does not cause total blindness as peripheral vision remains intact. |
This table helps put the fundamentals in perspective, but it's also crucial to know that AMD isn't just one single condition.
The Two Forms of AMD
When you're trying to understand what is macular degeneration, you need to know about its two main types. They both affect the macula, but they do so in very different ways, at different speeds, and require completely different approaches to manage them.
The two forms are:
- Dry AMD: This is the one you hear about most often and is thankfully the less severe form. It progresses very slowly, usually over many years.
- Wet AMD: This version is much less common but far more serious. It can move aggressively, causing rapid and severe vision loss if it isn't treated right away.
This infographic really helps visualize how common each type is.
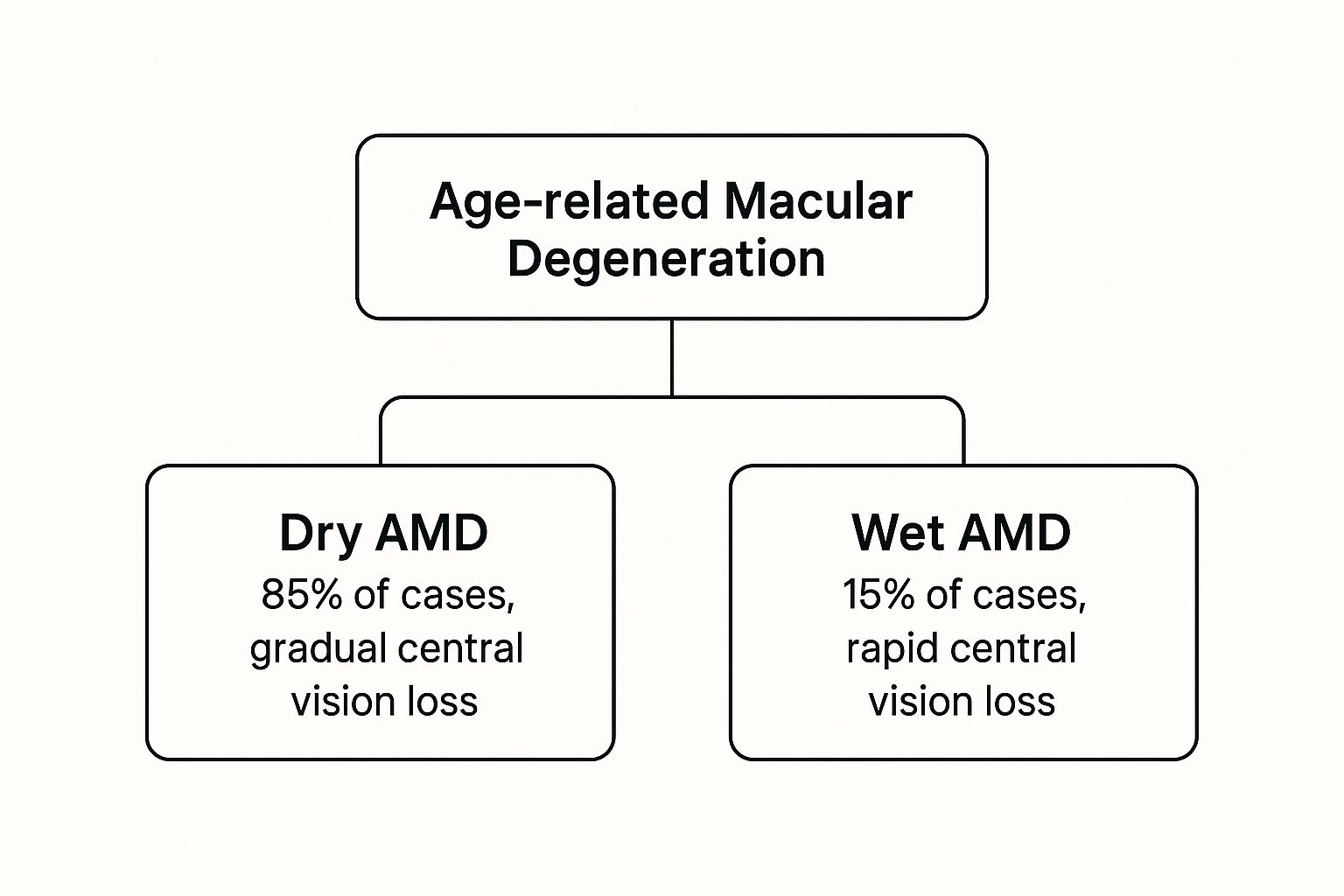
As you can see, Dry AMD makes up the vast majority of cases, which is a good thing since the more aggressive Wet AMD is much rarer.
A Growing Global Concern
Macular degeneration isn't just a minor issue; it's a major public health concern that's growing as the global population gets older. It’s one of the leading causes of vision impairment around the world.
Back in 2021, it was estimated that about 3.40 million males and 4.66 million females had vision impairment because of AMD. And those numbers are on the rise. Projections show they could jump to 5.82 million males and 7.54 million females by 2030. If you're interested, you can dive deeper into the data on global AMD prevalence.
The core takeaway is that AMD selectively targets your central vision—the vision you rely on for detail-oriented tasks. It’s like looking at a photograph where the main subject is blurry, but the background remains perfectly clear. Grasping this distinction is the first step toward understanding the condition's true impact.
Understanding Dry vs Wet Macular Degeneration
While "macular degeneration" sounds like a single diagnosis, it actually unfolds in two very different ways. Getting to know the difference between its "dry" and "wet" forms is the key to understanding how AMD progresses and why treatments are so distinct.
They might share a name, but their impact on your vision and the speed at which they develop are worlds apart. The vast majority of people diagnosed with AMD have the dry version.
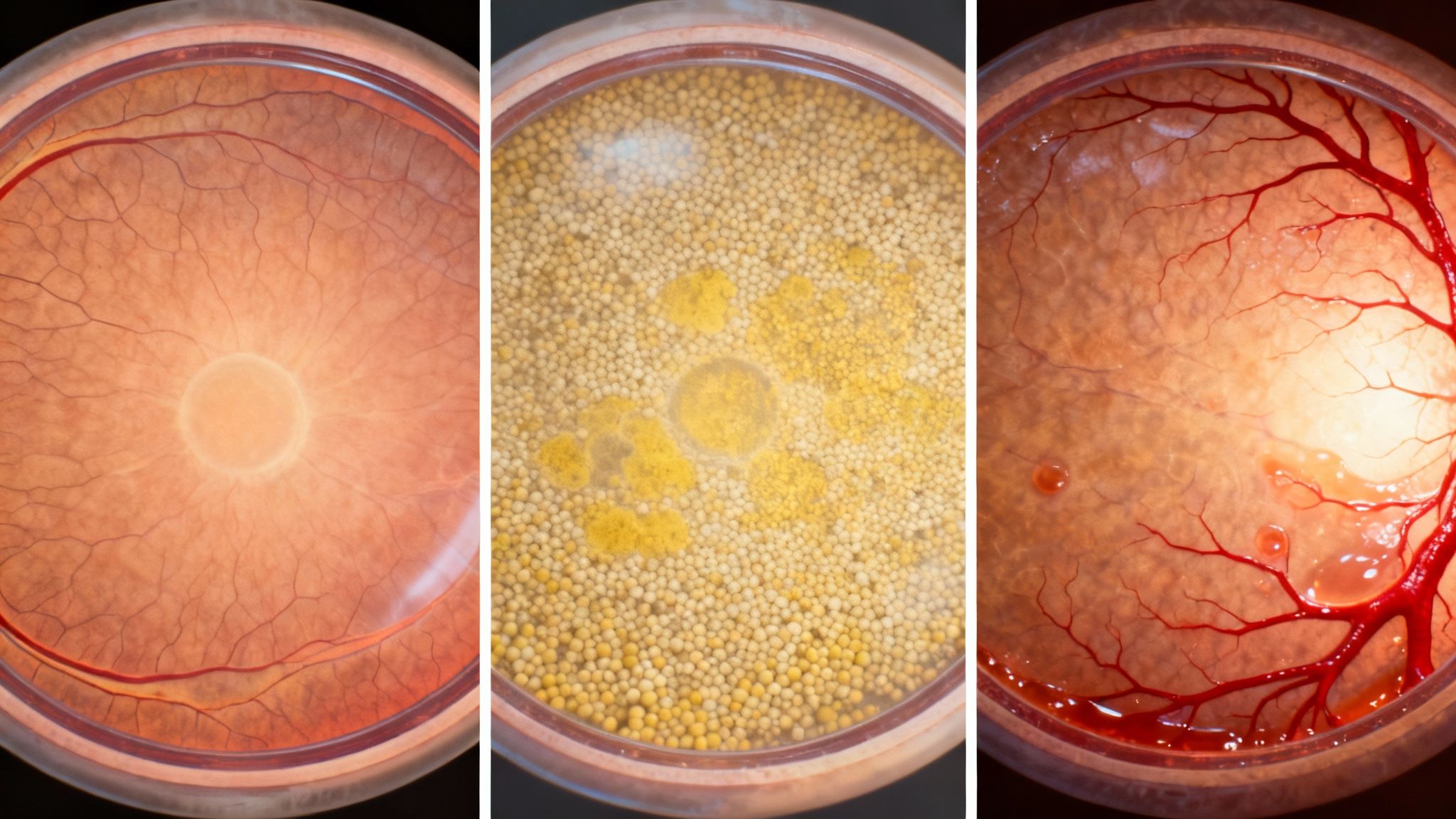
Imagine an old photograph slowly fading over time. The details get hazy, the colors lose their pop, and the whole image just gradually loses its sharpness. That’s a pretty good picture of what happens to your central vision with dry AMD.
It's a slow burn, caused by the thinning of the macula and the buildup of tiny yellow protein deposits called drusen. As these bits of cellular debris accumulate and the macular tissue wears down, your central vision gets dimmer and less defined over many years.
This is a massive global health issue. An estimated 200 million people worldwide were living with AMD in recent years, and that number is projected to climb to nearly 288 million by 2040. Dry AMD makes up about 90% of these cases, while the more aggressive wet form accounts for the other 10%. You can dig into more statistics on the global impact of AMD.
The Slow Fading of Dry AMD
The progression of dry AMD is often so subtle that many people don't notice it at first. The brain is pretty clever at compensating for minor vision loss, so the changes can fly under the radar for a long time.
Over the years, though, the effects become more obvious. You might find yourself needing brighter light to read, or notice that colors look washed out. Eventually, a blurry spot can pop up right in the center of your vision, making it tough to recognize faces or read a line of text.
Here are the key takeaways for dry AMD:
- Slow Progression: Vision loss happens gradually over several years.
- Drusen Buildup: The presence of those yellow deposits is a hallmark sign.
- Macular Thinning: The light-sensitive cells in the macula slowly break down.
- High Prevalence: It's by far the most common form of the condition.
While we don't have a cure for dry AMD, managing it revolves around slowing it down. This usually involves specific nutritional supplements and lifestyle changes aimed at preserving vision for as long as possible and preventing it from turning into the more severe wet form.
The Sudden Attack of Wet AMD
Now, let's talk about the other side of the coin. If dry AMD is a fading photograph, wet AMD is like a sudden pipe burst under your floorboards—it’s aggressive, fast-moving, and can cause serious damage in a very short amount of time.
This "leak" in the eye happens when fragile, abnormal blood vessels start growing underneath the macula. The medical term for this is choroidal neovascularization (CNV), but all you really need to know is that these new vessels are weak and leaky. They ooze blood and fluid directly into the retina.
This leakage causes rapid and severe damage to the macula. It leads to distorted vision—where straight lines suddenly appear wavy—and the abrupt appearance of a dark blind spot right in your central field of view.
Here's what defines wet AMD:
- Rapid Onset: Vision loss can happen fast, sometimes over just days or weeks.
- Abnormal Blood Vessels: New, leaky vessels grow where they shouldn't.
- Fluid Leakage: Blood and fluid seep into and damage the macular cells.
- Severe Vision Loss: It's responsible for about 90% of all legal blindness caused by macular degeneration.
Even though wet AMD is much less common, its potential to steal sight makes early detection and immediate treatment absolutely critical. Getting help right away can stop the leakage and, in many cases, preserve or even bring back some of the vision that was lost.
Recognizing Early Symptoms And Warning Signs
Macular degeneration is sneaky. It often begins with subtle changes you might brush off as just being tired or needing a new glasses prescription. But catching these early warning signs is the single most powerful thing you can do to protect your vision.
The symptoms almost always pop up right in your central field of view, while your peripheral (side) vision stays completely normal. The real challenge is that our brains are incredibly good at compensating for small visual hiccups, so you might not even realize something’s off until the condition has already started to progress.
Seeing The World Differently
The visual shifts from AMD aren't just about simple blurriness. The condition can warp how you perceive the world in some very specific ways. Think less about clinical terms and more about what you might actually notice day-to-day.
Here are the most common early signals:
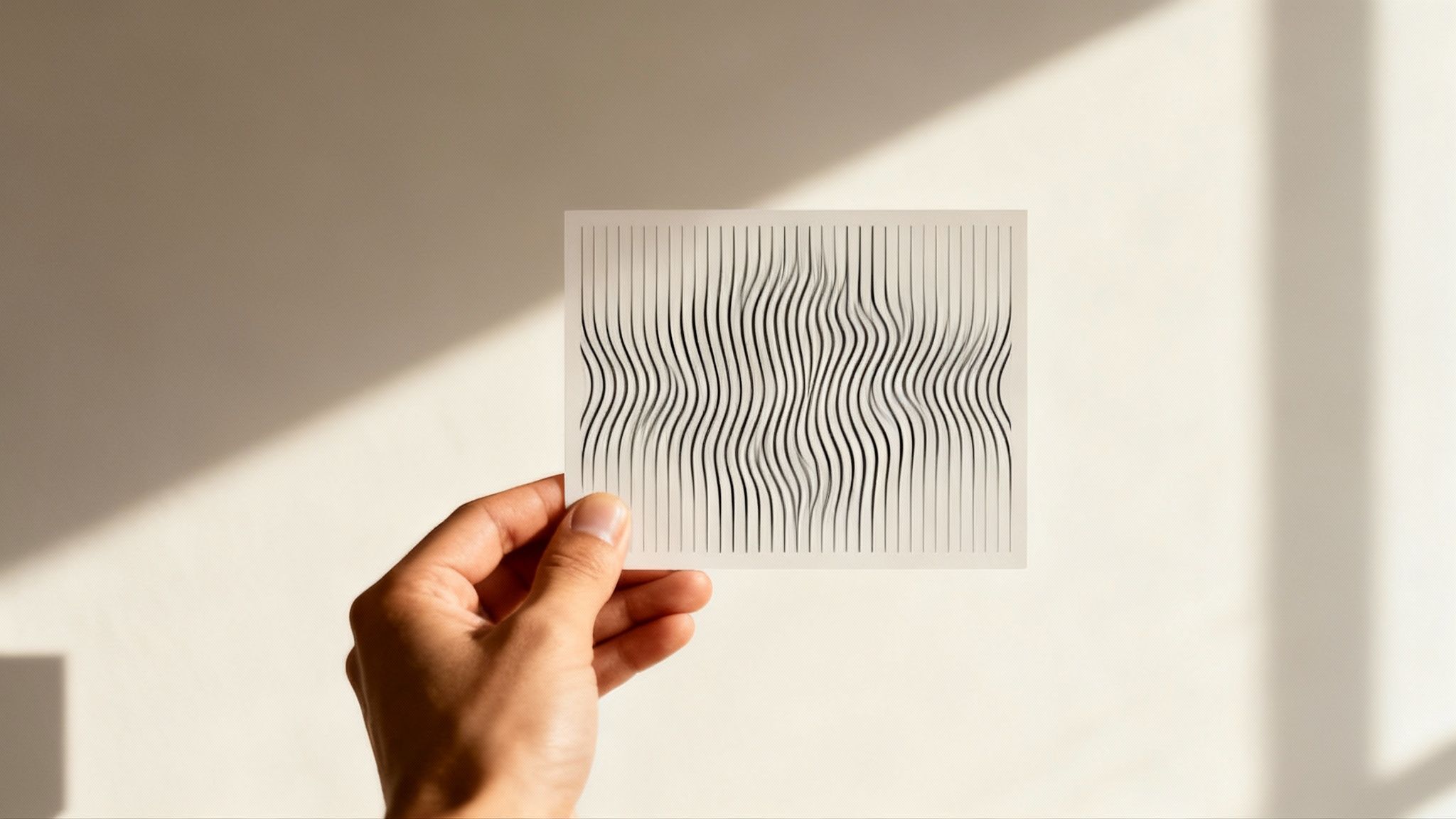
- Distorted Lines (Metamorphopsia): This is a big one. Straight lines—like a doorframe, window blinds, or the grout on a tile floor—can suddenly look wavy, bent, or crooked. It’s often one of the first and most telling signs, especially for wet AMD.
- A Blurry or Dark Spot: A persistent dark spot or smudge might appear in the center of your vision. It can feel like a fingerprint on your glasses that you just can’t seem to wipe clean.
- Faded Colors: You might notice that colors just don't seem as bright or vibrant as they used to. A brilliant red stop sign might look dull, or you could have a hard time telling similar shades apart.
- Trouble with Details: Recognizing faces across a room, reading fine print, or doing any task that requires sharp, detailed vision can become a real struggle.
These signs are your eyes sending a clear message that something is happening with your macula. Paying attention is the key to getting the prompt care you need.
Your At-Home Vision Check: The Amsler Grid
You don't have to wait for your annual eye exam to keep tabs on your vision. One of the simplest and most effective tools for catching early AMD-related changes is the Amsler grid. It’s just a basic pattern of straight lines with a dot in the center, like a piece of graph paper.
Using it is simple and takes less than a minute.
- Put on your regular reading glasses and hold the grid about 12-15 inches away—a comfortable reading distance.
- Cover one eye completely.
- With your uncovered eye, stare directly at the dot in the center.
- While looking at the dot, notice the lines around it. Ask yourself: Do any lines look wavy, blurry, or distorted? Are there any missing spots or dark areas on the grid?
- Now, switch eyes and repeat the test.
Think of the Amsler grid as an early warning system. Doing this quick self-check once a week can help you spot any new or worsening distortions, giving you a clear signal that it's time to call your eye doctor right away.
If you notice any changes at all, it's crucial to schedule an appointment with your ophthalmologist immediately. Early detection, particularly for wet AMD, is your best shot at getting treatments that can slow the disease down and preserve your precious central vision for years to come.
Key Risk Factors And What You Can Control
When we talk about what macular degeneration is, it helps to understand why some people get it and others don't. Think of it like a puzzle—some pieces are fixed from the start, but you have the power to swap out quite a few others. Certain risk factors are just part of your personal blueprint, but many are tied directly to lifestyle choices you make every single day.
Figuring out which is which is the first step toward taking charge of your long-term eye health. It’s all about recognizing what you can’t change and pouring your energy into the powerful, proactive steps that protect your vision.
Factors You Cannot Change
Some risk factors are simply out of your hands. These are the genetic and biological cards you’ve been dealt.
- Age: This is the single biggest one. The odds of developing AMD jump significantly after you hit 50. It’s right there in the name: age-related macular degeneration.
- Genetics and Family History: If a close relative—like a parent or sibling—has AMD, your own risk can shoot up by as much as 50%. Scientists have linked specific genes to the condition, making family history a major clue.
- Race: Caucasians tend to have a higher rate of macular degeneration when compared to people of African or Hispanic descent.
You can't turn back the clock or rewrite your DNA. But knowing you have these predispositions just makes it that much more important to get a handle on the risks you can control.
The Most Significant Controllable Risk Factor Smoking
If there is one thing—and only one thing—you do to lower your risk, it should be quitting smoking. Tobacco use is, without a doubt, the most significant lifestyle choice you can change to protect yourself from AMD. In fact, smokers are up to four times more likely to develop the condition than non-smokers.
Smoking is brutal on the tiny, delicate blood vessels in your retina. It also unleashes oxidative stress, which basically fast-forwards the aging process inside your macula. This damage adds up over time, so the longer and more heavily you smoke, the higher your risk climbs.
Quitting smoking is the single most impactful step you can take for your eye health. Research has shown that stopping can help delay the onset of advanced AMD, making it a critical choice for anyone serious about preserving their vision.
Lifestyle Choices That Matter
Beyond smoking, a handful of other daily habits play a huge part in keeping your macula healthy. These are the areas where making conscious choices can truly make a difference.
Diet and Nutrition What you put on your plate directly feeds your eyes. A diet loaded with specific nutrients can help shield the cells in your macula from damage. Try to pack your meals with:
- Leafy Greens: Spinach and kale are bursting with lutein and zeaxanthin, two antioxidants that are found in high concentrations in a healthy macula.
- Oily Fish: Think salmon, sardines, and trout. They’re rich in omega-3 fatty acids, which are fantastic for supporting overall retinal health.
- Colorful Produce: Brightly colored fruits and vegetables deliver a cocktail of essential vitamins that fight back against cellular damage.
Cardiovascular Health Your eyes aren't islands; they’re connected to your whole body through a vast network of tiny blood vessels. Things like high blood pressure, high cholesterol, and obesity can wreak havoc on these vessels, bumping up your AMD risk. Keeping a healthy weight and managing your blood pressure isn't just good for your heart—it's essential for your sight.
Sun Exposure Just like UV rays can burn your skin, they can slowly damage your eyes over a lifetime. Years of exposure to ultraviolet light and high-energy visible blue light are thought to contribute to retinal damage. A simple but powerful defense is wearing sunglasses that block 100% of UVA and UVB rays. For a deeper dive, check out our guide on how UV rays affect your eyes.
How Doctors Diagnose And Treat AMD
Getting a potential diagnosis of macular degeneration can feel pretty overwhelming. The good news is that understanding how doctors figure it all out can take away a lot of that uncertainty. Your ophthalmologist has a series of specialized, painless tests to get a crystal-clear picture of what's happening inside your eye, leading to a solid diagnosis and a plan to move forward.
The process usually kicks off with a comprehensive dilated eye exam. Your doctor will use special eye drops to widen your pupils. Think of it like opening the curtains on a window to get a better view of the room inside—in this case, the back of your eye. This lets them look closely at your retina and macula for any tell-tale signs of drusen (the classic sign of dry AMD) or any suspicious blood vessel growth.
Advanced Imaging for a Deeper Look
To really nail down a diagnosis and figure out the exact type and stage of AMD, doctors often bring in some high-tech imaging tools. These machines give them an incredibly detailed look at the layers of your retina, way beyond what the human eye can see on its own.
-
Optical Coherence Tomography (OCT): This is kind of like an ultrasound for your eye, but it uses light waves instead of sound. An OCT scan creates a high-resolution, cross-sectional map of your retina. This allows your doctor to measure its thickness and spot any fluid leakage or swelling that points toward wet AMD.
-
Fluorescein Angiography: If your doctor suspects wet AMD, this test is the gold standard for confirmation. A safe, yellow dye is injected into a vein in your arm, which quickly travels through your bloodstream to the vessels in your eye. A special camera then snaps photos as the dye circulates, lighting up any leaky or abnormal blood vessels hiding under the macula.
As technology gets smarter, so does our ability to spot and track diseases. For example, the use of AI for medical diagnosis is becoming more common in helping doctors interpret these complex images with even greater accuracy.
Modern Treatment Strategies for AMD
Once the diagnosis is clear, the focus shifts to treatment. While we don't have a full cure for AMD just yet, modern therapies are fantastic at slowing it down and protecting your precious central vision. The right approach is all about whether you have the dry or wet form of the condition.
For the intermediate stages of dry AMD, the main game plan is nutritional support. The landmark Age-Related Eye Disease Studies (AREDS and AREDS2) found a specific cocktail of vitamins and minerals that can make a real difference.
An AREDS2 formula, which you can get over-the-counter, packs high doses of Vitamin C, Vitamin E, lutein, zeaxanthin, zinc, and copper. For people at high risk, this supplement has been shown to lower the risk of dry AMD advancing to the more serious wet form by about 25%.
Revolutionizing Wet AMD Treatment
When it comes to wet AMD, the goal is to stop the leaky blood vessels causing all the trouble. Today, the standard of care is a class of drugs called anti-VEGF (anti-vascular endothelial growth factor) medications.
These incredible drugs work by blocking the protein that tells abnormal blood vessels to grow and leak. They're given through quick, virtually painless injections right into the eye. I know, that sounds terrifying, but the procedure is over in a flash, and your eye is completely numbed beforehand. These injections can stop wet AMD in its tracks and, in many cases, even bring back some of the vision that was lost.
The development of these treatments has been a total game-changer. You can see this reflected in the market; the global AMD drugs market size was valued at around USD 10.57 billion in 2024 and is projected to hit USD 29.04 billion by 2034. This boom is fueled by just how effective anti-VEGF shots are, along with exciting ongoing research into new biologics and gene therapies.
Living Well And Protecting Your Vision
Hearing you have macular degeneration is a big deal, no question. But it's far from the end of the story. Think of it as the beginning of a new, proactive journey—one where you take charge of protecting your vision and keeping your quality of life high. Empowering yourself with a few practical strategies can make a world of difference.
Many of these changes can start right at home. Simple tweaks, like improving the lighting in your living room or using high-contrast colors for things like light switches, can dramatically boost visibility and safety. And don't overlook low-vision aids like magnifiers, large-print books, or even voice-activated tech; they are fantastic for helping you keep up with hobbies and stay independent.
Adopting An Eye-Healthy Lifestyle
Your daily habits are a powerful tool in managing how AMD progresses. A great place to start is with an eye-healthy diet. You're essentially giving your macula the specific nutrients it needs to defend itself from damage.
- Load up on leafy greens: Spinach and kale are absolutely packed with lutein and zeaxanthin, two antioxidants that are found in high concentrations in a healthy macula.
- Eat oily fish: Think salmon, sardines, and trout. They are rich in omega-3 fatty acids, which are crucial for overall retinal function.
- Choose colorful produce: Brightly colored fruits and vegetables give you a wide array of vitamins that help protect your eyes.
Beyond what’s on your plate, it’s smart to get a full picture of your health. Checking your nutritional status with a blood test for vitamin and mineral deficiency can be a great proactive step, because what’s good for your body is good for your eyes. To dive deeper, you can also check out our guide to the best vitamins for eye health.
Shielding Your Eyes From Harmful Light
Protecting your eyes from environmental stress is just as critical as what you put into your body. Over a lifetime, the cumulative exposure to UV rays and high-energy visible (HEV) blue light—from both the sun and our screens—can add to retinal stress.
For anyone who spends a good chunk of their day looking at computers, tablets, or smartphones, filtering that blue light becomes a key part of your defense. This is where the right kind of eyewear can offer some real support for your long-term eye health.
We recommend PROSPEK glasses as an excellent option. They are specifically designed to filter the most harmful wavelengths of blue light, which can help reduce digital eye strain and support the delicate cells of your macula.
When you combine an eye-healthy diet, smart adjustments around the house, and protective measures like blue light filtering glasses, you really start to take control of your environment. These are fundamental steps to living well, holding onto your independence, and protecting your precious sight for years to come.
Frequently Asked Questions About AMD
When you or a loved one is diagnosed with macular degeneration, it's natural to have a lot of questions. Getting clear, straightforward answers can give you peace of mind and help you understand the journey ahead. Here are some of the most common questions we hear about AMD.
Can Macular Degeneration Be Cured?
Right now, there isn't a cure for AMD, but that absolutely does not mean there aren’t powerful ways to fight it. The treatments available today are incredibly effective at slowing down the disease and managing its impact on your vision. Early detection and staying on top of your treatment plan are the keys to the best possible outcome.
For dry AMD, taking AREDS2 nutritional supplements can dramatically lower the risk of it progressing to the more aggressive wet form. For wet AMD, anti-VEGF injections have been a true game-changer, stopping the leaky blood vessels in their tracks and, in some cases, even bringing back some lost vision.
Will I Go Completely Blind From AMD?
This is a huge fear for many people, but the short answer is that macular degeneration almost never causes total blindness. This condition specifically targets your central vision—the detailed, straight-ahead vision you rely on for reading, driving, and recognizing faces.
Your peripheral (side) vision is typically left untouched. While AMD can lead to legal blindness and make certain activities very difficult, you'll still be able to navigate your surroundings and maintain a degree of visual independence, often with the help of low-vision aids. It also helps to know how different eye conditions work; for instance, you can learn more about another common issue in our guide on what glaucoma is and how it can be treated.
How Often Should I Get My Eyes Checked?
Think of regular, comprehensive eye exams as your first line of defense. For adults over 50 with no known risk factors, most eye care professionals recommend an exam every one to two years.
But if you have known risk factors—like a family history of AMD or if you're a current or former smoker—your doctor will almost certainly want to see you for annual check-ups. Once a diagnosis of AMD is made, your ophthalmologist will create a personalized schedule to monitor your eyes closely.
This kind of proactive monitoring is what allows your doctor to catch any changes the moment they happen, opening the door for timely treatment that can preserve your sight for many years to come.
At Spektrum Glasses, we're dedicated to supporting your long-term eye health with advanced lens technology. Our premium blue light blocking glasses are designed to reduce digital eye strain and protect your vision in a screen-filled world. Explore our collection at https://www.spektrumglasses.com.
